Dr Shayani wrote an article explaining the increased access to bariatric surgery, and its relation to the Affordable Care Act. The article was published in the SouthTown Star, and has been reprinted here. Please contact Dr Shayani if you have any questions about bariatric surgery.
Changes pave way for increased access to bariatric surgery
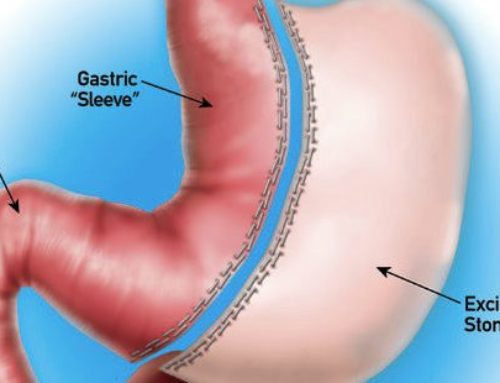
Bariatric, or weight loss, surgery is often a critical component of care for morbidly obese patients.
Until recently, the Centers for Medicare and Medicaid Services (CMS) provided coverage only for those surgeries performed at Bariatric Surgery Centers of Excellence.
The Center of Excellence requirement, which previously had been largely determined on volume-based criteria, meant that most patients had to travel some distance if they chose to have weight loss surgery.
In challenging the requirement, a group of prominent surgeons from Michigan revealed there is no data to support better outcomes at accredited versus non-accredited institutions. The biggest difference was, in fact, cost, which is much lower at local hospitals.
Upon performing their due diligence, the CMS reversed their Center for Excellence requirement. This decision underscores their belief in bariatric surgery for the management of morbidly obese patients. Moreover, it illustrates a belief that good results can be obtained when well-trained surgeons in local, community hospitals, such as Franciscan St. James, perform the procedure.
Most importantly for patients, the reversal provides greater access to much needed care.
Bariatric Surgery a Critical Tool
Medical management of morbid obesity, which involves following a rigid, lifelong regimen, results in sustained weight loss for five to 10 percent of patients at best. Bariatric surgery, however, has a success rate of approximately 75 to 80 percent.
Now recognized as a disease, morbid obesity predisposes people to an array of health conditions. Among more commonly known comorbidities are high blood pressure, diabetes and sleep apnea. Other, lesser known conditions include infertility, bladder and bowel incontinence and the increased incidence of breast and colon cancers.
Once patients lose a significant amount of weight, most see dramatic improvements in those related medical conditions.
Many are better able to manage their diabetes and no longer require medication. Those with sleep apnea may be able to stop using their CPAP masks and machines, and others find their blood pressure has returned to normal with no need to continue medication.
The Affordable Care Act
If the new Affordable Care Act (ACA) works as planned, we can assume most people will be insured within three years, and the new law will prohibit insurers from dropping people who are morbidly obese.
Presently, bariatric surgery is not included in mandatory coverage in all policies but it’s believed that pressure from medical and surgical societies will change that. These societies include entities such as the American Society for Metabolic and Bariatric Surgeons, the American Diabetic Association, the American Heart Association and many others who firmly believe there’s a place for bariatric surgery in the spectrum of care we offer to morbidly obese patients.
As minimum coverage policies are phased out, which appears to be a goal, it is our hope bariatric surgery will be covered in all U.S. policies by 2015.
In fact, it is strongly believed that following weight loss surgery, insurers quickly recoup the cost of bariatric surgery.
Studies have shown a return on investment begins after two or three years. Policies that have captive members for long periods of time, such a Medicare and Medicaid and large insurers like Kaiser Permanente, have concluded it is wise to cover the procedure.